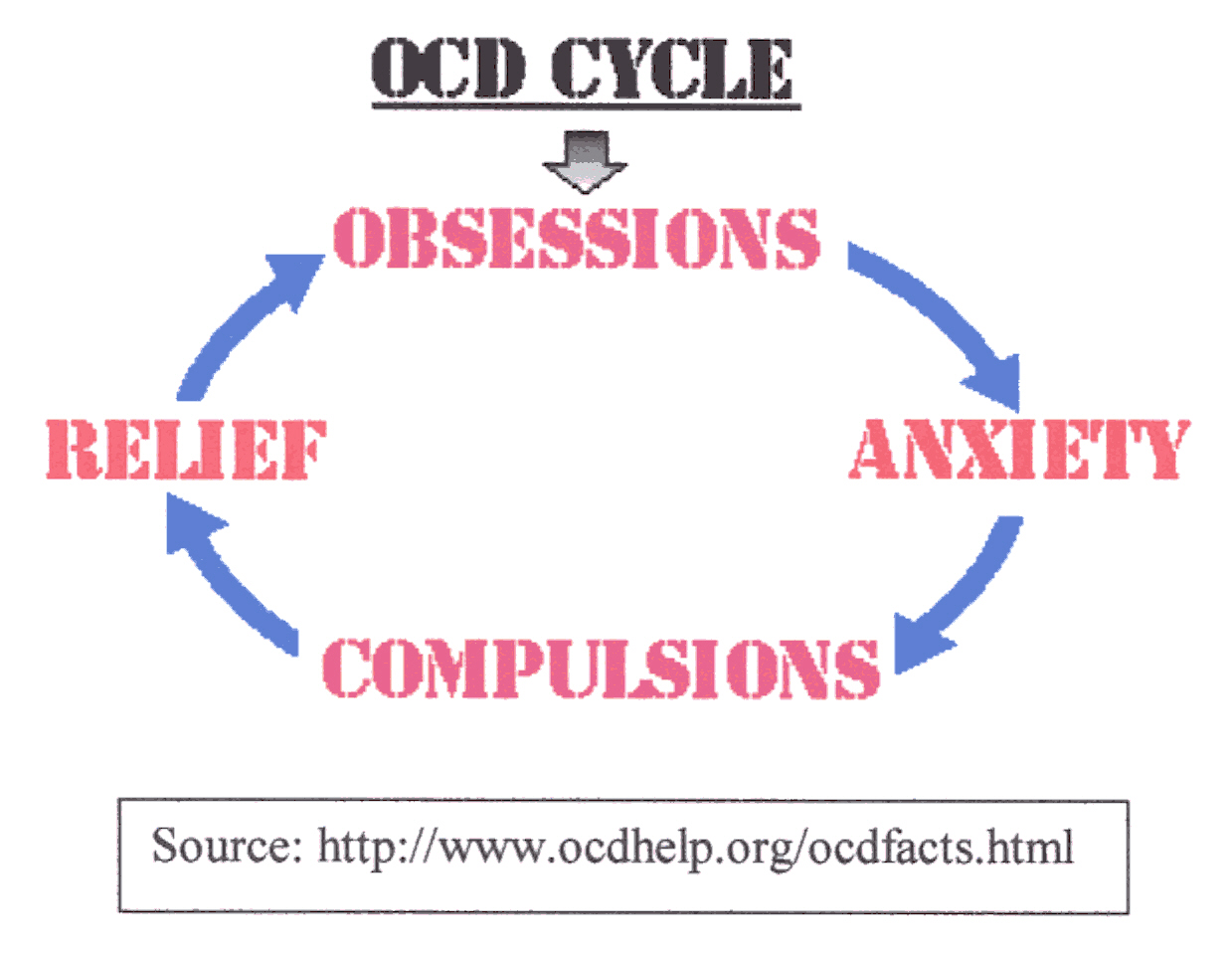
| There are several key features of OCD. Obsessions are unwanted ideas, disturbing thoughts, or impulses such as fear of contamination from germs, or fear that one might accidentally harm a loved one. These obsessions often produce great anxiety. To deal with this overwhelming anxiety, a person with OCD often resorts to repetitive behaviors called compulsions. Some of the most common compulsions are washing, checking, hoarding, and repeating (1). The compulsions are often mental problems such as list making, counting, or repeating words or phrases(2). These obsessions and compulsions make up the OCD cycle. The person has obsessions that cause anxiety and to alleviate the anxiety, the person acts out the compulsions. The rituals provide temporary relief but often the symptoms worsen(1). People with OCD often recognize the irrationality of their obsessions and compulsions and they do not derive pleasure from their rituals. Because of their understanding of the senselessness of their actions, people with OCD often try to suppress their thoughts or resist from compulsive behavior(2). However, overtime the anxiety is often too much to handle and the symptoms are ultimately manifested; sometimes to the point that the rituals are so time consuming that the person is not able to function. | 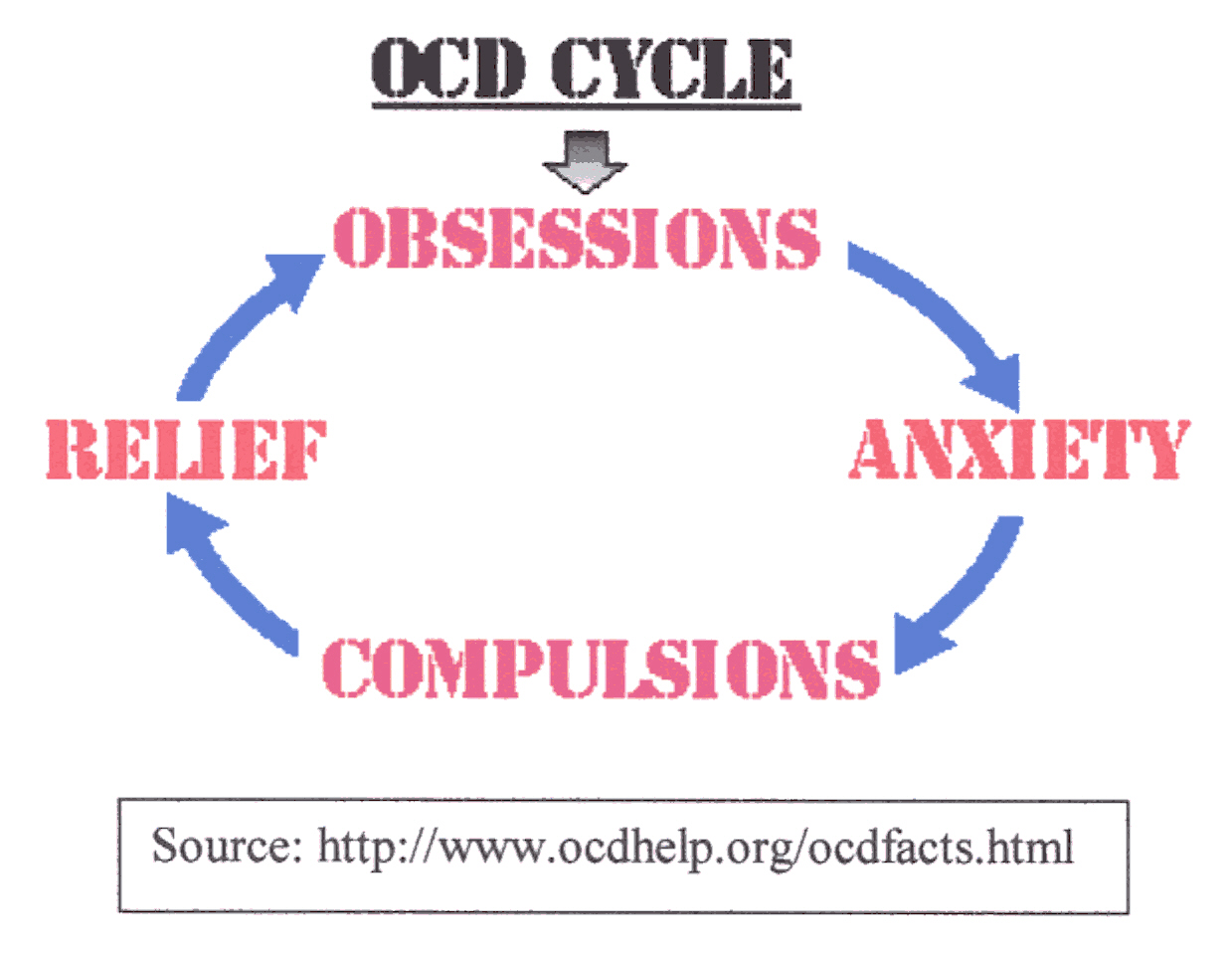 |
Despite the prevalence of OCD, little is known about what actually causes
the disorder. There are several theories that try to justify this illness.
Stress does not cause OCD, but it may lead to the onset of symptoms(1).
An early theory that has just about been abandoned said that OCD was caused
by life experiences such as abuse. A second theory that does have some
validity is heredity. Perhaps a person's genes carry a predisposition to
OCD. In fact, 15 to 20 percent of sufferers have immediate family members
with the same disease(3). More recent evidence suggests
that OCD may be triggered by a streptococcal infection. Some children develop
a complication called Sydenham's chorea and OCD-like symptoms that develop
in days or weeks, but not all the symptoms characteristic of chorea (such
as jerky movements) arise(4). Susan Swedo, a neuroscientist
at the National Institute of Mental Health, called this condition PANDAS,
or pediatric autoimmune neuropsychiatric disorders associated with streptococcus(4).
It has been shown that children with Syndenham's chorea produce antibodies
to fight the bacteria. These antibodies mistakenly attack the caudate nucleus(4).
There are two other theories that I will examine further, the brain abnormality
theory and the chemical imbalance theory.
 |
Some researchers think that obsessive-compulsive disorder is associated with abnormalities in the frontal cortex and basal ganglia regions of the brain. Also, certain studies have found that people with OCD have significantly less white matter in the brain than control subjects(5). Thus, there is probably less communication in parts of the brain than in normal people. Lewis Baxter of the UCLA Center for Health Science showed that there were higher rates of metabolic activity in the frontal cortex of the brain of people with OCD than control subjects(6). Interestingly, other regions that deal with anxiety such as the hippocampus and temporal cortex seem to function normally in people with OCD(7). Jeffrey Schwartz, of the UCLA School of Medicine, used positron-emission tomography (PET) scans to show where the brain is metabolically most active in OCD patients. His team was able find which parts of the brain were most |
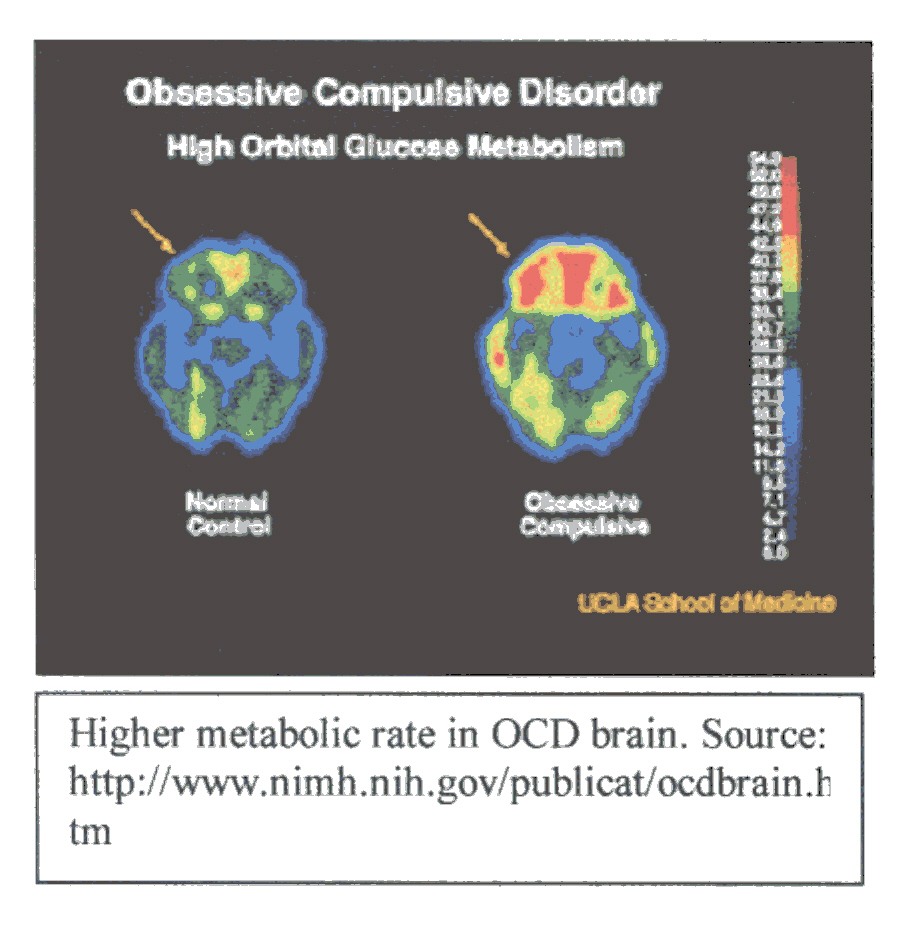
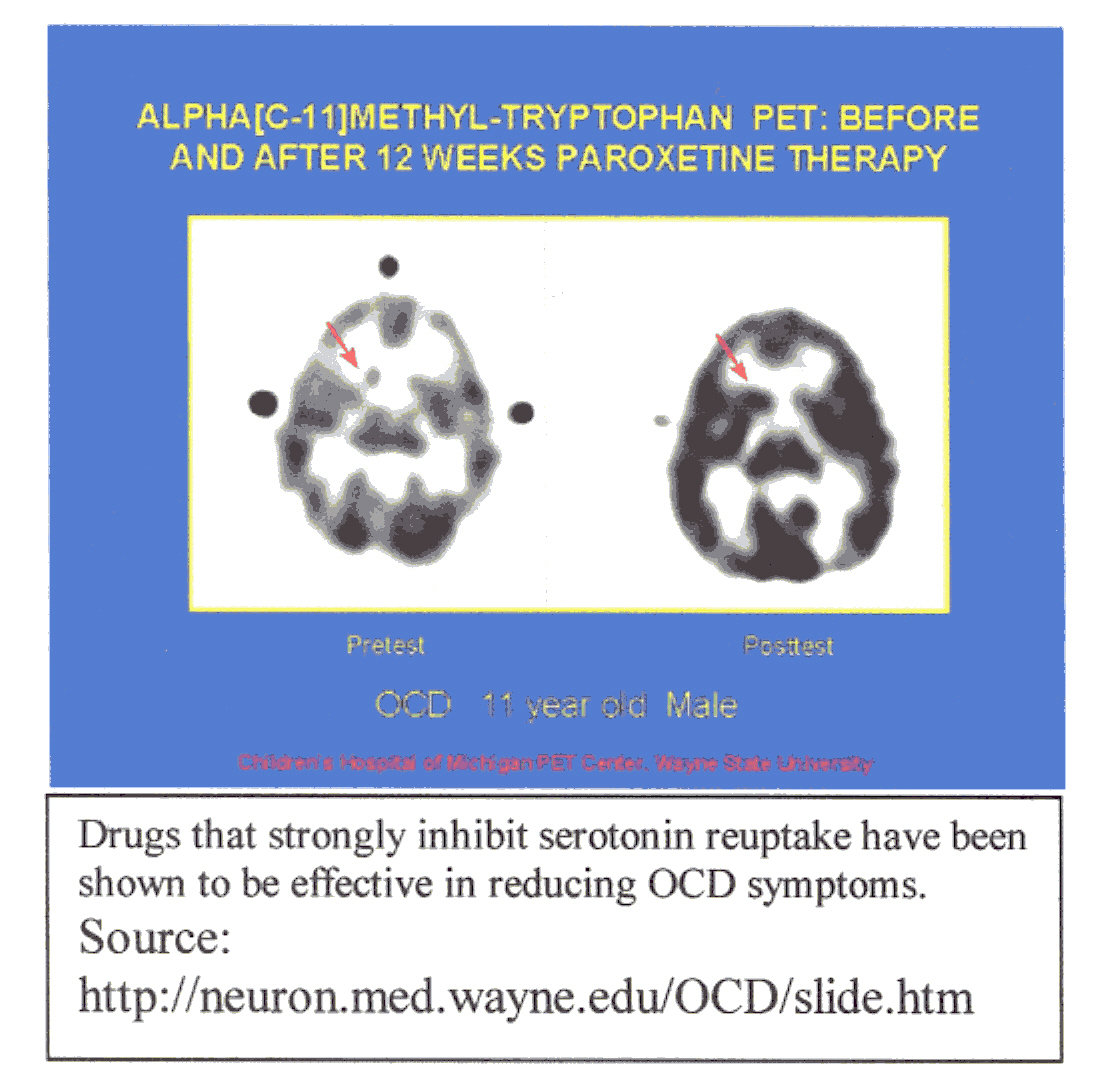
The chemical imbalance theory suggests that low levels of serotonin,
a neurotransmitter, may cause obsessive-compulsive disorder(9).
Studies indicate that low levels of serotonin in the synapse may contribute
to OCD(9). Drugs that affect serotonin reduce symptoms
of OCD(10). In over 75 percent of patients, these drugs
are effective. The group of drugs that affects serotonin are called Selective
Serotonin Reuptake Inhibitors (SSRIs), which include fluvoxamine (Luvox),
fluoxetine (Prozac), paroxetine (Paxil), citalopram (Celexa), and sertraline
(Zoloft)(11). All SSRIs essentially work in the following
manner: when nerve A fires a signal to nerve B, neurotransmitters are released
and cross the synapse and fit into receptors in nerve B. The serotonin
is on one side of the synapse and thus spreads out and some go back to
the other side where they are taken back into nerve A. Eventually all of
the serotonin returns to nerve A's side. In OCD there is not enough serotonin.
SSRIs fit into the reuptake sites of nerve A and thus not all of the neurotransmitter
goes back to nerve A and some serotonin remains in the synapse. Nerve A
produces more serotonin to compensate for what it was not able to recover.
Eventually enough serotonin is produced that the communications are able
to work properly(12). PET scans made at the Children's
Hospital of Michigan PET Center, Wayne State University show lower serotonin
levels in OCD patients than control subjects. Another PET scan shows that
with SSRIs, the PET scan of an OCD patient after treatment looks more like
the scan of the control subject's brain(13).
We began this course discussing whether the brain equals behavior. It was mentioned that if this were so, then all behavior is controlled and caused by the brain. What if we put a new twist on the question: can behavior control the brain? A type of OCD treatment produces a chemical change in the brains of patients who undergo this treatment. The specific behavior therapy that alleviates OCD is called "exposure and response prevention."(10) The patient willingly confronts the fear either directly or by imagination. The patient is encouraged to refrain from the rituals. The program continues on a step-by-step basis depending on the patient's ability to tolerate the anxiety and refrain from rituals(6). As therapy continues, the patient is better able to handle the anxiety and refrain from compulsions. In a recent study of 300 patients who were treated with therapy, 76 percent still showed significant relief from three months to six years after treatment(6). MRI and PET scans have confirmed that the chemistry of the brain is influenced by the therapy. From the examination of certain treatments of OCD, our assertion that the brain, or more precisely, the nervous system equals behavior is supported.
2)Key Features of OCD, This site offers a brief explanation of several characteristics of OCD
3)) Biological Bases of Obsessive Compulsive Disorder, Explanation of some biological theories of OCD
4)Over and over and over and over ·Over and over and over and over· , A short description of the history of OCD and a discussion of the findings of certain PET scans. Also, many possible causes of OCD are discussed.
5)What Causes OCD? , Possible theories of the cause of OCD
6)Obsessive-Compulsive Disorder , Answers common questions about OCD
7)Obsessive Compulsive Disorder: An Assessment of Etiology and Treatment , This site explains possible causes of OCD and it examines certain treatments of the disorder
8)The Chemistry of Obsession , Describes the findings of certain brain imaging techniques and explains a possible cause of OCD
9) Biological Theory , Introduces three theories about the causes of OCD
10)Treatment of OCD , Describes two types of treatment for OCD
11)OCD Medication: Adults , Answers to questions concerning medications used to treat OCD.
12)Response to Inquiry about SSRIs , This article offers an explanation of how SSRIs might work.
13)Obsessive
Compulsive Disorder Clinical Research Program , A slide presentation
of pictures of brain scans with descriptions of each slide.